 Herniated Disc
Herniated Disc
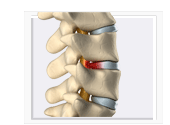
A herniated disc (also known as slipped disc, bulging disc, or ruptured disc) is a rupture of the outer casing of the disc. Discs are shock-absorbing cushions separating the vertebrae. Discs have a tough outer coating and a jelly-like inner substance. Discs don't actually slip out of place - they are firmly attached to the vertebrae. A disc can, however, bulge out beyond its normal position and the outer casing can tear or rupture. This is called a herniated disc.
The lumbar spine is the most common location for a herniated disc as the lower back is subject to the most mechanical stress and supports most of the weight of the body.
Symptoms
When a disc is ruptured some of the inner substance protrudes and may irritate or compress the spinal nerve roots. If this occurs in the lumbar spine, it may cause sciatica - pain and/or numbness that radiates from the lower back, through the buttocks, back of the leg, and sometimes to the foot. The pain can vary, from a burning sensation or a dull ache. It may be intermittent or chronic. The severity of the pain can range from mild to severe. In some cases, there may not be any symptoms. If a herniated disc occurs in the neck area (cervical spine), pain, tingling and weakness may occur in the arm or hand.
*Always consult a doctor for pain that spreads down your leg or is accompanied by tingling, numbness or weakness.
When a nerve is compressed it is often referred to as a "pinched nerve." While a herniated disc is the most common cause of a "pinched nerve" in the lower spine, other conditions such as spinal stenosis, swelling of surrounding tissues due to muscle injury, and bone spurs that may occur in osteoarthritis of the spine may compress spinal nerve roots.
Is there a difference between a herniated disc and a bulging disc?
These terms are often used interchangeably; both are often used as catchall descriptions for an abnormality of a disc. The term bulging disc is usually used to describe a disc that bulges slightly and does not produce symptoms. A herniated disc is usually used to describe a disc that protrudes against a spinal nerve root and causes pain. However, some bulging discs bulge enough to cause problems and some herniated discs do not cause any problems.
Definition of a bulging disc: Sometimes the disc does not actually rupture but bulges due to a weakening of the outer part of the disc that lets the inner fluid to push against the weakened wall and cause a bulge.
Bulging discs are considered a normal part of aging. Bulging discs often cause no problems, but if a bulging disc protrudes against a spinal nerve root, back pain can result. A bulging disc is more susceptible tearing, and becoming a herniated disc.
Definition of a herniated disc: A herniated disc is a rupture of the outer casing of the disc. The inner substance of the disc then protrudes.
Causes/Risk Factors and Prevention
A Herniated Disc Can Develop Gradually or Occur SuddenlyA herniated disc may occur suddenly by the excessive compression of the disc from a fall or car accident or lifting a heavy object.
Gradual degenerative changes in the discs that occur over a long period of time make the discs susceptible to injury. Even when a herniated disc has developed gradually, the symptoms may appear suddenly.
Disc Degeneration
With aging, the discs lose some flexibility and water content, and may develop cracks and fissures These changes leave the discs less able to handle compression and more likely to bulge or rupture. As the contents of the discs continue to "dry out" the risk of a herniated disc actually decreases but disc degeneration may eventually cause other problems (osteoarthritis of the spinal joints, spinal stenosis).
Genetics and lifestyle also play a role in disc degeneration. Some people have more brittle discs than others of the same age. Smokers have more disc damage on average than non-smokers. Spending most of the day sitting may contribute to gradual degenerative changes to discs in the lumbar spine.
Activities and herniated disc
Over time, activities that involve excessive forward bending and lifting (especially with a rounded back) may contribute to degeneration of the discs in the lumbar spine, which make the discs more vulnerable to rupture.
Repetitive bending and/or lifting are hard on the lower back. Bending forward from a standing or sitting position makes the lower back muscles to work much harder to support the weight of the upper body and the discs in the lumbar spine compress more under the extra load. Lifting a heavy object adds to the load on the lower back and increases the risk of rupturing a disc in the lumber spine (and, more commonly, of straining lower back muscles).
Bending forward with a rounded back (bending forward from the waist) is much worse than bending forward with a neutral back (pivoting forward from the hips). It causes more compression at the front of the disc and more pressure at the back of the disc as the contents of the disc are forced backward
Lack of Exercise and herniated disc
Core muscles must have enough strength and endurance to maintain neutral alignment of the spine, which reduces the load to the spinal discs and joints. Strengthening exercises are essential to counteract the gradual loss of muscle mass that comes with aging. Low-impact aerobics also increase core muscle endurance and help keep the discs hydrated.
Body WeightBeing overweight increases the load on the lower back and increases compression of the discs in the lumber spine. Even small reduction in body weight can make a difference.
Posture and herniated discThe discs are under even pressure when the spine is in neutral alignment. When the natural curve of the lower back is increased (sway back) or decreased (flattened back) the discs in the lumbar spine are more compressed at the back or front of the discs. This excessive compression on one side of the disc causes gradual damage to the disc and increases the risk of herniated disc.
Treatment / Pain Relief
*See a physician immediately if pain radiates down your leg, or is accompanied by tingling, numbness or weakness to rule out serious conditions that may require immediate surgery.
Since most herniated discs improve without surgery (the protruding part of the disc may gradually shrink), the focus is on treating the pain and any inflammation. Once the pain and other symptoms have resolved, exercises can help prevent a reoccurrence.
Medications
NSAIDs (anti-inflammatory medications) such as aspirin and ibuprofen are often helpful, especially during the first few days after an acute injury. Stronger prescription pain medications may be needed for severe pain. Muscle relaxants are sometimes prescribed after an acute injury as muscles contract in response to inflammation.
The use of heat and cold : Ice is used during the acute phase to reduce inflammation and pain. Ice is most useful for the first couple of days when inflammation is worse. Do not use heat on an acute injury as it increases inflammation. When the initial pain and inflammation have subsided often after 4 or 5 days heat can be used or heat and cold can be alternated. If an activity has caused pain to quickly flare up, ice can be helpful. Heat increases blood flow to an area, which promotes healing. Heat also relaxes the muscles.
Spinal traction is not recommended for acute lower back pain but may relieve sciatica caused by a herniated disc in the lumbar spine.
Exercise
Be sure to seek a proper diagnosis and an exercise plan from your physician or physical therapist.
Muscles often contract around the site of pain. Stretching exercises and/or massage therapy can help release muscle spasms and pain. Do not do stretches that involve bending forward from a standing or sitting position is you have a herniated disc in the lower back - or do any exercise that worsens the symptoms.
Low-impact aerobic exercise such as walking and swimming help keep the discs hydrated and nourished and promote healing. Low-impact aerobics also increase endurance of the core muscles. Strong core muscles protect and support the spine in proper alignment but strengthening exercises should not be attempted until advised by a physician or physical therapist (usually after most of the pain and other symptoms have resolved). Do not do any exercise or activity that worsens pain.
Avoid activities that increase symptoms
Any movement or activity that increases symptoms of pain or numbness should be avoided. If the herniated disc in the lumbar spine, avoid activities stress the lower back such as bending forward and lifting. Avoid rounding the back as it causes uneven compression of the discs in the lumbar spine and puts pressure on the back of the disc - towards the spinal nerve roots. Bending forward with a rounded back is worse than either alone (including exercises that involve forward bending from a sitting or standing position).
Sitting places more pressure on the discs in the lower back than standing. Avoid sitting for long periods of time. Take frequent breaks from sitting. A chair that reclines slightly shifts the body weight to the backrest of the chair and takes some stress off of the discs in the lower spine.
Maintain proper posture.
While sitting maintain the normal inward curve in the lower back. If the pelvis is allowed to tilt backward, the normal curve in the lower back is lost. The vertebrae in the lumber spine become closer together at the front and push the contents of the discs backward towards the spinal nerves. Sitting on a wedge cushion helps to prevent the pelvis from tilting backward.
A medium-firm mattress will help keep the spine in proper alignment while sleeping.
Invasive Treatments
Spinal injections may be used when severe radicular pain does not respond to non-invasive treatments. A mixture of corticosteroids (a powerful anti-inflammatory) and a local anesthetic is used in spinal injections. There are rare but serious risks involved.
Pain relief often lasts from between a few weeks to few months. Many people experience relief from one injection, others may need up to three. If no pain relief at all is obtained from the first injection, no more are usually given.
A selective nerve block is an injection given near the nerve root that appears to be causing the pain where it exits the spinal column.
An epidural steroid injection is an injection of steroids and a local anesthetic into the epidural space (the space between the membrane covering the spinal cord and the wall of the spinal canal).
Surgery does not guarantee pain relief. In the time it takes to recover from surgery, most herniated discs will have improved without any treatment. Though surgery is usually a last resort, if there are signs of progressive nerve damage (e.g. progressive weakness), waiting too long to have surgery may result in permanent nerve damage.
*If nerves that affect bladder or bowel control are affected, immediate surgery is necessary to prevent permanent nerve damage.
Fortunately, the vast majority of herniated discs improve without surgery.
A herniated disc is not nearly as common a cause of lower back pain as muscle or ligament strain.
